Scientists Just Deleted the Extra Chromosome That Causes Down Syndrome Using CRISPR
Last updated on
Down syndrome, also known as trisomy 21, occurs when a person is born with an extra copy of chromosome 21. This additional genetic material changes how cells function and develop, leading to a range of health challenges. These can include differences in learning and memory, congenital heart defects, thyroid disorders, and an increased risk of certain conditions such as Alzheimer’s disease. Current treatments focus on managing these complications and supporting overall health, but they do not address the extra chromosome itself. A recent study from Mie University in Japan has shown that it is possible to remove this extra chromosome from human cells in the laboratory using CRISPR-Cas9, a precise gene-editing technology. The research, led by Ryotaro Hashizume, demonstrated that by designing CRISPR to target only the surplus chromosome, scientists could restore the cells to a more typical genetic state. This resulted in changes in gene activity and cell function that brought them closer to what is seen in cells without trisomy 21.
Targeting the Genetic Cause
Down syndrome is caused by the presence of an extra copy of chromosome 21, a condition known as trisomy 21. This additional chromosome changes how cells function at a very fundamental level. It disrupts normal gene expression, leading to differences in brain development, altered metabolism, and increased risks for a range of health issues, including heart defects, thyroid problems, and early-onset Alzheimer’s disease. These effects occur because the extra chromosome increases the activity of certain genes beyond normal levels, which in turn changes how proteins are made and how cells carry out basic processes. For decades, treatment approaches have focused on managing the symptoms and complications of Down syndrome rather than addressing this underlying genetic cause. While medical care, early interventions, and supportive therapies have improved quality of life, the genetic basis has remained untouched — until now. A research team in Japan, led by Ryotaro Hashizume at Mie University, has successfully removed the extra chromosome from human cells grown in a laboratory using CRISPR-Cas9 gene-editing technology. This process, called trisomic rescue, involves designing CRISPR guide molecules that specifically target only the extra chromosome 21 without interfering with the normal pair. CRISPR-Cas9 acts like a molecular tool that can recognize an exact DNA sequence and cut it, allowing scientists to remove unwanted genetic material. By tailoring the system to focus exclusively on the surplus chromosome, the researchers were able to restore the cells to a more typical genetic state without introducing major damage to the rest of the genome. Once the extra chromosome was removed, the results were significant. The edited cells began showing normal patterns of gene activity and protein production. Genes linked to nervous system development — often suppressed in Down syndrome — became more active, while metabolic genes that tend to be overactive slowed down. This was the first time scientists have used CRISPR to remove an entire chromosome from human cells, demonstrating that it is possible to address the root cause of trisomy 21 at a cellular level. While this work is still in the laboratory phase and not yet applicable in medical treatment, it marks an important shift from treating symptoms toward potentially correcting the source of the condition.How Cell Function Improved
The removal of the extra chromosome had a clear impact on how the cells behaved. Edited cells grew faster and divided more efficiently than the unedited trisomic cells. This change in growth rate is meaningful because carrying extra genetic material puts cells under a constant state of stress, slowing down their ability to function normally. By eliminating the extra chromosome, the researchers relieved some of this stress, allowing the cells to operate more efficiently. The treated cells also produced fewer reactive oxygen species — unstable molecules that can damage DNA, proteins, and cell membranes, and are linked to aging and chronic disease. Lowering these harmful byproducts suggested that the cells’ mitochondria — the parts of the cell that generate energy — were working more effectively. Improved mitochondrial function means better overall energy production and less cellular damage over time. Importantly, the research team achieved these results not only in stem cells but also in mature skin fibroblasts taken from individuals with Down syndrome. Stem cells are known for their ability to divide and develop into different cell types, so editing them is more straightforward. Mature cells, on the other hand, are fully developed and do not divide as readily, making them harder to edit. Successfully removing the extra chromosome in both types shows that this approach could potentially be applied across different tissues in the body. If adapted for cells that do not divide at all — such as many brain and muscle cells — this technique could eventually support therapies for tissues that were previously thought to be beyond genetic correction. Gene activity changes after editing were consistent with what scientists already know about the biology of Down syndrome. The restored activity of brain-related genes could, in theory, improve the development and function of the nervous system. At the same time, the reduction in overactive metabolic genes could help reduce the strain on the body’s systems. These combined effects suggest that removing the extra chromosome could have a broad impact on health, potentially reducing multiple complications at once rather than addressing them individually. While much more research is needed to see how these changes play out in living systems, the lab results provide a strong basis for further investigation.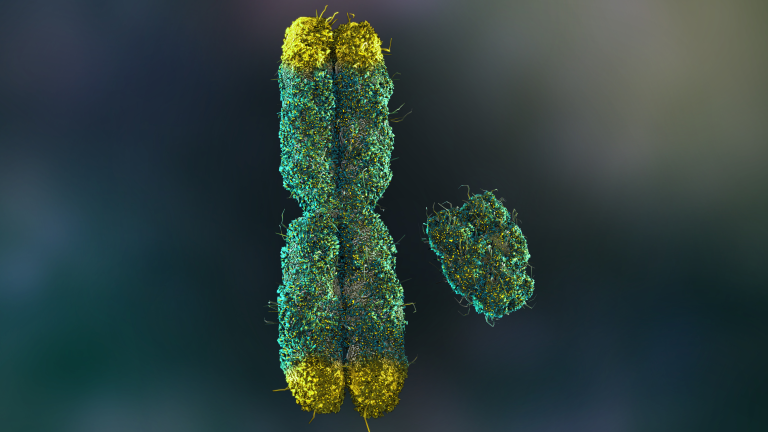
Potential Uses and Current Limitations
Successfully removing the extra chromosome in a lab setting creates new possibilities for regenerative medicine. In the future, corrected cells could be used to grow healthy tissue for transplants, repair damaged organs, or replace malfunctioning cells in individuals with Down syndrome. This could also help reduce the risk of associated conditions such as congenital heart defects, thyroid disease, gastrointestinal issues, and Alzheimer’s disease, which affect many people with the condition. By working at the genetic level, this approach could theoretically improve multiple aspects of health at once, rather than focusing on one symptom or complication at a time. However, these possibilities are still far from becoming a clinical reality. One of the main challenges is precision. Although the CRISPR system was designed to target only the extra chromosome 21, some cuts occurred in normal chromosomes. These unintended changes could lead to harmful side effects, making safety a major concern. The researchers are now refining the CRISPR guide molecules to make them more accurate and to ensure they do not bind to the wrong parts of the genome. Another challenge is understanding how edited cells behave over the long term. Even if they appear normal at first, changes in gene expression or cell function could occur months or years later, and these must be carefully studied before any clinical use is considered. Moving from laboratory work to patient treatment will involve solving several technical and logistical problems. Scientists would need to develop safe and effective methods for delivering CRISPR into the right cells inside the body, and they would need to ensure that the chromosome removal process works reliably in those cells. Regulatory approval for such a therapy would also require extensive testing in animal models and multiple stages of human clinical trials. Each of these steps will take years, if not decades, to complete, so while the breakthrough is important, it is still the starting point for a long process.
Ethical Considerations
The ability to remove the genetic cause of Down syndrome raises questions that extend beyond the laboratory. While the scientific aim may be to reduce medical complications and improve health, there is concern about how such technology could affect societal attitudes toward people with the condition. In Iceland, for example, Down syndrome has become rare due to widespread use of prenatal screening and subsequent abortion decisions, a trend that has led to international debate. Critics argue that such practices can send a message that lives with Down syndrome are less valued, which can have social and psychological impacts on individuals and families. Astridur Stefansdottir, a professor in applied ethics at the University of Iceland, has pointed out that many people with Down syndrome, as well as their families, find developments aimed at reducing the prevalence of the condition to be troubling. These concerns highlight the importance of involving those directly affected in discussions about how genetic technologies should be used. While the Japanese research team has stated that their goal is not to eliminate Down syndrome from the population but to address specific health challenges, the potential for unintended social consequences remains. Bioethicists recommend that conversations about genetic editing should happen alongside scientific development, not after the technology is ready for use. This means policymakers, scientists, healthcare providers, people with Down syndrome, and their advocates should work together to set clear guidelines. Such collaboration can help ensure that the use of powerful tools like CRISPR is guided by a combination of scientific knowledge, medical benefit, and respect for diversity.
Looking Ahead
The work by the Mie University team shows that it is possible to remove an entire chromosome from human cells using CRISPR, expanding the potential applications of gene editing beyond single-gene changes. This development opens new avenues for research into genetic conditions and could eventually change how certain disorders are treated. For Down syndrome, it offers a proof-of-concept that the root genetic cause can be targeted directly, something that was previously considered unattainable. The next stage of this research will focus on improving precision, ensuring long-term stability of the edited cells, and exploring safe ways to deliver the CRISPR system in living organisms. It will also require an ongoing public dialogue about how such technology should be applied. The medical potential is significant, but so is the responsibility to ensure that it is used in a way that balances health benefits with ethical considerations.
Some of the links I post on this site are affiliate links. If you go through them to make a purchase, I will earn a small commission (at no additional cost to you). However, note that I’m recommending these products because of their quality and that I have good experience using them, not because of the commission to be made.

































 JOIN OVER
JOIN OVER
Comments