The Quiet Rise of Thyroid Cancer Among Younger Women
Last updated on
Thyroid cancer is becoming one of the most unsettling medical trends of our time. The numbers climb even as medical technology improves, and the shift is not happening in the demographic most people would expect. Younger women are increasingly facing a disease once linked mostly with aging. Many discover it only after months or years of fatigue, voice changes or a small lump they dismissed as stress or thyroid imbalance. This quiet rise has puzzled researchers, doctors and public health experts across the world. Science paints a picture that is both hopeful and cautionary. Thyroid cancer is usually treatable and survival rates remain high, yet the story behind why cases are growing is more complex than simple overdiagnosis or routine screening. A web of factors that include environmental exposures, metabolic changes, advances in imaging and even subtle hormonal differences between genders appears to be influencing this trend. Beneath the data sits a deeper message about modern health and how our bodies respond to the pressures of contemporary life. Understanding why this is happening requires more than a quick look at symptoms or statistics. It asks us to examine the interaction between environment, physiology and lifestyle, while also acknowledging how early signs often blend into the everyday noise of life. For young women balancing work, family and rising social stress, that subtlety can become a dangerous kind of camouflage.The Rising Trend in Thyroid Cancer
Thyroid cancer is growing faster than many other cancers. In the United States, cases tripled between nineteen eighty and twenty sixteen. The pattern is similar in many countries that do not have large scale screening programs. This recent rise surprised experts because there were no nuclear disasters or mass radiation exposures during the decades when numbers escalated. The thyroid sits at the base of the neck and controls metabolism, energy, heart rate and temperature. When cells within the gland begin to multiply uncontrollably, they form tumors that may remain slow growing or begin to spread. Papillary thyroid cancer is the most common type and usually grows slowly. Other types like follicular, medullary and the rare anaplastic form behave very differently and may spread earlier or resist treatment.
Why Young Women Are Most Affected
The gender difference is striking. Women develop thyroid cancer three times more often than men. The most affected age range is women in their thirties, forties and fifties, years when busy schedules and constant demands can make subtle symptoms easy to ignore. Men usually develop thyroid cancer later in life, most often in their sixties or seventies. Hormonal influences likely play a major role. The thyroid is deeply tied to the endocrine system, which is the network of glands that produce and regulate hormones. Women experience monthly hormonal cycles, pregnancy related hormone shifts and changes during perimenopause. These natural rhythms create more opportunities for thyroid stress or imbalance. Thyroid nodules are incredibly common in women. Up to eighty percent may develop them during their lifetime. While only a small percentage are cancerous, this creates a larger pool of cases that require attention and screening. A small lump, a change in voice or a bit of trouble swallowing can blend into daily stress or aging and feel unimportant until symptoms start to grow.
Subtle Symptoms That Go Unnoticed
The early signs of thyroid cancer are often so soft they blend into normal life. This is one reason young women miss them or interpret them as stress, exhaustion or the result of a packed schedule. Common early signs include:-
- Lump or swelling in the neck
-
- Voice changes or hoarseness
-
- Difficulty swallowing or the sensation of pressure in the throat
-
- Persistent fatigue that does not improve
-
- Unexplained weight loss
Overdiagnosis Versus True Increase

Obesity and Metabolic Stress
One of the strongest links in current research is the connection between high body mass index and thyroid cancer. Individuals with high BMI are more likely to develop thyroid cancer and more likely to be diagnosed with advanced tumors. Obesity also increases levels of thyroid stimulating hormone, a chemical produced by the pituitary gland that influences thyroid function. Inflammation, insulin resistance and metabolic stress are all potential drivers. These conditions alter cellular behavior and may increase the likelihood of mutations within thyroid tissue. This is especially concerning because obesity rates began rising around the same time thyroid cancer rates increased. Many researchers now believe obesity contributes to the rise in cases, worsening tumor behavior and supporting the development of more aggressive forms. This does not replace environmental explanations but adds another layer to a complex picture.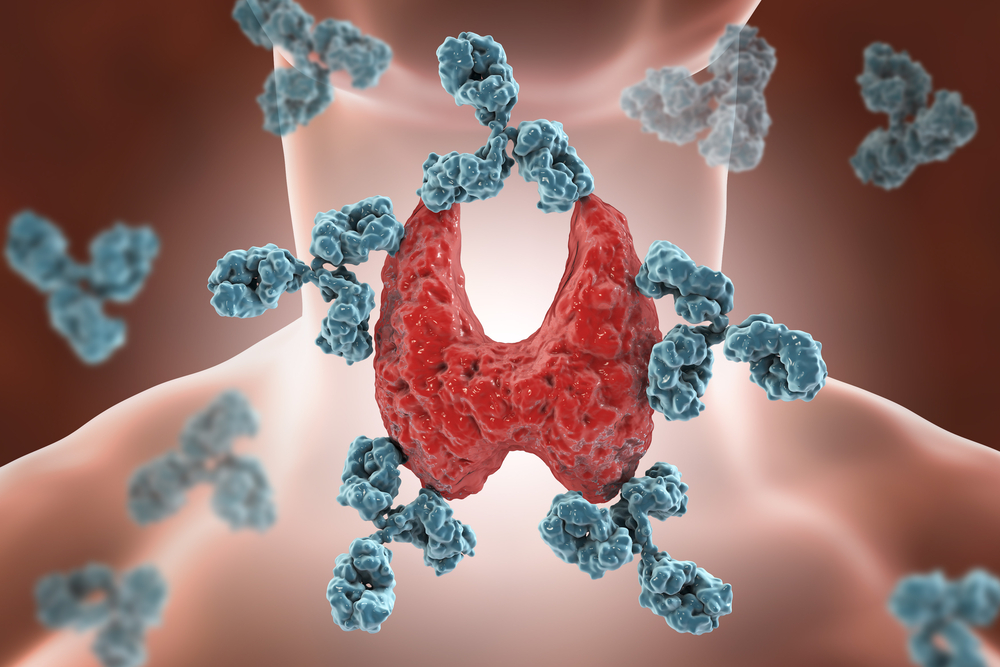
Environmental Exposures and Chemical Disruptors
Thyroid function is highly sensitive to chemicals in the environment. Endocrine disrupting chemicals, often found in cookware, personal care products, carpeting, plastics, pesticides and food packaging, mimic hormones or block natural hormonal activity. Substances like PFOA and PFOS have drawn attention due to potential links with thyroid disease. The evidence is mixed but concerning. Even weak chemical effects can become significant over years of exposure. Our bodies were not designed to continuously encounter synthetic chemical signals, and the thyroid seems especially vulnerable to this disruption. Another theory involves trace elements found in volcanic soils. Countries with volcanic activity sometimes have higher thyroid cancer rates. These environments may contain elevated levels of metals that influence thyroid function. While evidence is still limited, research continues.Medical Radiation and Childhood Exposure

How Thyroid Cancer Is Diagnosed Today
Diagnosis begins with physical examination, lab tests and imaging. Ultrasound remains one of the most important tools because it reveals the structure and behavior of thyroid nodules. When a nodule looks suspicious, a doctor performs a fine needle biopsy to examine cells under a microscope. Most biopsies identify benign nodules. A smaller percentage confirm cancer, and some remain unclear. In these cases doctors rely on additional imaging, genetic testing and monitored follow up. Accuracy in diagnosis has improved significantly. Skilled interpretation of imaging and biopsy results can change a patient’s entire treatment path. There have been cases where a second biopsy or a reevaluation of imaging revealed a missed diagnosis, saving the patient from delayed treatment.Treatment Approaches and New Innovations

The Emotional Journey for Women
Toward Better Awareness and Prevention
The quiet rise of thyroid cancer among young women is not a simple problem, and prevention is still challenging because the causes are multifactorial. Even so, awareness has a powerful role. Recognizing subtle symptoms and responding early can change the outcome dramatically. Regular checkups, attention to hormonal changes, careful use of medical imaging and understanding personal risk factors all support earlier diagnosis and stronger healing. Women who trust their instincts often discover issues long before tests reveal them.Where Awareness Meets Action
Thyroid cancer is rising for reasons that reflect the complexity of modern life. Improved imaging uncovered many harmless nodules, but deeper forces like metabolic stress, environmental exposures, hormonal patterns and increased radiation from medical scans are influencing more aggressive cases. The burden falls most heavily on young women whose lives are already full of demands that disguise the early signs. Science continues to evolve and treatment improves every year. Most thyroid cancers remain highly treatable and survival rates are extraordinary. The real challenge lies in recognizing the quiet symptoms, understanding the invisible pressures that shape thyroid health and empowering women to advocate for their bodies even when the signs seem small. This rise is not a story of fear. It is a reminder that the body always communicates, even in whispers, and those whispers matter.Some of the links I post on this site are affiliate links. If you go through them to make a purchase, I will earn a small commission (at no additional cost to you). However, note that I’m recommending these products because of their quality and that I have good experience using them, not because of the commission to be made.

































 JOIN OVER
JOIN OVER
Comments