This New ‘universal cancer vaccine’ trains the immune system to kill any tumor
Last updated on
A research team at the University of Florida has developed an experimental mRNA vaccine that could fundamentally change how cancer is treated. Unlike existing cancer vaccines that target a single tumor type or require customization for each patient, this “universal” approach is designed to work against any cancer by boosting the immune system’s ability to detect and attack tumors. In preclinical studies, it not only enhanced the effects of standard immunotherapy drugs but, in some cases, eliminated tumors on its own.
The technology builds on the same principles used in COVID-19 mRNA vaccines but adapts them for a different goal: making cancer cells more visible to the immune system. Early results in animal models are promising, suggesting that one day this vaccine could offer a widely accessible alternative or complement to surgery, chemotherapy, and radiation. While human trials are still ahead, the research points toward a future where fighting cancer could become faster, less invasive, and more effective across a broad range of patients.
How the “Universal Cancer Vaccine” Works
Researchers at the University of Florida have developed an experimental mRNA-based vaccine designed to help the immune system recognize and attack cancer cells—regardless of the cancer type. Unlike traditional cancer vaccines, which target a specific protein found in a particular tumor, this approach trains the immune system to mount a broad, virus-like defense against tumors in general.
The vaccine uses lipid nanoparticles to deliver strands of messenger RNA (mRNA) into the body, similar to the delivery method used in COVID-19 vaccines. Instead of carrying instructions to make a viral protein, the mRNA directs cells to produce proteins—such as PD-L1—that are found in cancer cells but often hidden from immune surveillance. By increasing PD-L1 expression within tumors, the vaccine effectively makes them more visible to the immune system. This primes immune cells, especially T cells, to target and destroy cancer cells.
This generalized immune activation proved successful in mouse studies, where the vaccine not only worked alongside existing immunotherapy drugs—such as PD-1 checkpoint inhibitors—to overcome drug-resistant melanoma, but in some cases, cleared tumors without any additional treatment. The strategy moves away from the two dominant approaches in cancer vaccine research—targeting common tumor markers or tailoring a vaccine to each patient’s tumor—and instead focuses on boosting the immune system’s overall readiness to fight cancer.
As Dr. Duane Mitchell, a co-author of the study, explained, this method could make an “off-the-shelf” cancer vaccine possible, eliminating the need for complex customization while still delivering a potent anti-tumor response.

How This Breakthrough Fits into Cancer Treatment Trends
For decades, the mainstays of cancer treatment have been surgery, chemotherapy, and radiation therapy. While these approaches have saved countless lives, they often come with significant side effects and, in many cases, the cancer still returns. Over the last 20 years, immunotherapy has emerged as a powerful fourth pillar of treatment. By training the body’s own immune system to recognize and attack tumors, therapies like checkpoint inhibitors and CAR-T cells have transformed outcomes for some patients, particularly in cancers like melanoma and certain blood cancers. However, these treatments are far from universal—many patients do not respond, and tumors can find ways to evade immune attack.
Personalized cancer vaccines have been one way researchers have tried to overcome these limitations. These vaccines are custom-designed for each patient based on the genetic mutations in their tumor. While promising in theory, the process is labor-intensive, expensive, and slow, which limits its accessibility and practicality for widespread use. The newly developed mRNA-based universal vaccine offers a fundamentally different strategy. Instead of tailoring treatment to a specific cancer marker, it uses a generalized approach to stimulate a robust immune response, enabling the body to target cancer cells regardless of their specific mutations.
Preclinical studies suggest that this universal approach may work both as a complement to existing treatments and as a stand-alone therapy in certain cases. For example, when combined with PD-1 checkpoint inhibitors—a standard immunotherapy—the vaccine helped overcome resistance in melanoma that had stopped responding to treatment. In other mouse models of brain, skin, and bone cancers, it sometimes eliminated tumors without any other intervention. This level of versatility is rare in oncology research and could make the vaccine a central part of treatment strategies in the future.
Why PD-L1 Targeting Matters
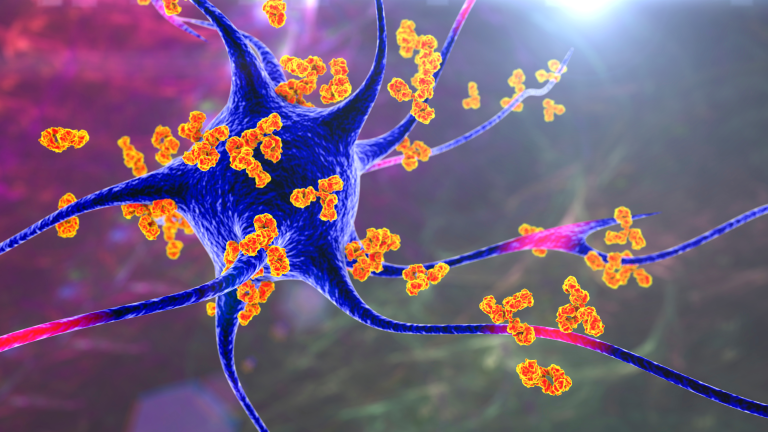
One of the most effective ways tumors protect themselves from immune attack is by using the PD-1/PD-L1 pathway. PD-L1 is a protein found on the surface of some cancer cells. When it binds to PD-1 receptors on T cells—immune cells responsible for killing infected or abnormal cells—it sends a “stand down” signal, essentially telling the immune system to leave the tumor alone. Checkpoint inhibitor drugs work by blocking either PD-1 or PD-L1, allowing T cells to stay active and attack the tumor. However, this approach only works if the tumor is already expressing PD-L1, which is not always the case.
The universal cancer vaccine changes this equation by inducing PD-L1 expression directly inside tumors, even in those that previously lacked it. This makes the cancer cells more visible to immune cells and allows checkpoint inhibitors to be more effective. By creating these “tags” on the tumor, the vaccine sets up the immune system for a much stronger response, both in combination with existing drugs and on its own.
This strategy has broad implications because it is not tied to one cancer type. Tumors from different tissues often use similar immune evasion tactics, so an approach that forces PD-L1 expression could, in theory, apply across many cancer types. That’s why researchers believe this could be a foundation for a truly universal cancer vaccine—one that doesn’t require tailoring to the genetics of a single patient’s tumor but still provokes a powerful and targeted immune attack.

Current Limitations and Next Steps in Research
While the results so far are promising, it’s important to recognize that this vaccine has only been tested in animal models. Human biology is more complex, and many therapies that work in mice do not translate directly to people. Before this can be considered for clinical use, researchers need to conduct phased human trials to confirm safety, determine optimal dosing, and measure effectiveness in real-world patient populations. There are also unanswered questions about how long the immune boost from the vaccine will last and whether repeated doses would be necessary.
The development process will also need to address potential safety concerns. Because the vaccine broadly stimulates the immune system, there is a possibility of triggering overactive immune responses or inflammation in healthy tissues. Regulators will require robust safety data before approving such a treatment. However, mRNA technology offers an advantage here—its flexibility allows researchers to adjust the formulation relatively quickly if problems arise, much like the rapid adaptation seen with COVID-19 vaccine updates.
The research team at the University of Florida is already working on refining the current mRNA formulations, experimenting with different delivery methods, and exploring how the vaccine performs against cancers known for their immune resistance, such as pancreatic and ovarian cancers. If early human trials produce strong safety and efficacy data, there may be opportunities to speed up development by leveraging the same manufacturing and regulatory pathways established for COVID-19 mRNA vaccines. Even with acceleration, experts caution that it will likely be several years before the vaccine is widely available.
Supporting Your Immune System While Awaiting New Therapies
Although a universal cancer vaccine could one day change the treatment landscape, it is not yet available outside of research settings. In the meantime, there are evidence-based steps that individuals can take to help maintain immune function and reduce overall cancer risk. These measures are not a substitute for medical treatment, but they can support the body’s natural defenses and complement regular medical care.
First, staying up to date on recommended cancer screenings is critical. Screenings such as mammograms, colonoscopies, Pap tests, and low-dose CT scans for high-risk smokers can detect cancers early, when they are most treatable. Second, nutrition plays a key role in immune health. Diets rich in fruits, vegetables, whole grains, legumes, and lean proteins provide the vitamins, minerals, and antioxidants the immune system needs to function effectively.
Regular physical activity is another important factor. Studies show that moderate exercise, such as brisk walking for 30 minutes most days, can improve immune regulation and lower inflammation—both important in cancer prevention and recovery. Avoiding tobacco and limiting alcohol are also well-established steps for reducing cancer risk and supporting immune function. Finally, managing chronic conditions such as diabetes, hypertension, and obesity can help prevent the suppression and systemic inflammation that often accompany these diseases.

Takeaway and Call to Action
The development of an mRNA-based universal cancer vaccine represents a potential shift in how we approach cancer treatment. Instead of creating separate vaccines for each cancer type or each individual patient, researchers may soon have a way to train the immune system to recognize and attack tumors of any kind. By exposing tumors through induced PD-L1 expression, this approach not only enhances the effectiveness of existing treatments like checkpoint inhibitors but also has the potential to work independently in eliminating cancer.
This innovation builds on decades of immunology research and the recent acceleration of mRNA technology through the global rollout of COVID-19 vaccines. If clinical trials confirm its effectiveness in humans, it could lead to faster, more accessible, and less invasive cancer treatments, potentially replacing or reducing the need for chemotherapy, radiation, or surgery in some cases.
For now, the most impactful actions individuals can take are to stay informed through reliable sources, follow established cancer prevention guidelines, and consider participation in clinical trials if eligible. Public awareness and involvement in research are essential in moving breakthroughs like this from the laboratory into everyday medical practice.
Some of the links I post on this site are affiliate links. If you go through them to make a purchase, I will earn a small commission (at no additional cost to you). However, note that I’m recommending these products because of their quality and that I have good experience using them, not because of the commission to be made.
































 JOIN OVER
JOIN OVER
Comments