NHS launches world-first cancer blood test to speed up personalised treatment and avoid invasive biopsies.
Last updated on
For patients facing a cancer diagnosis, the path to treatment can be fraught with delays, uncertainty, and invasive procedures. But a quiet revolution is unfolding within the NHS that could change that reality for thousands each year. In a world-first move, NHS England is rolling out a groundbreaking blood test, known as a liquid biopsy, designed to detect cancer-related genetic mutations from a simple blood sample. This test marks a transformative shift in how certain cancers, including lung and advanced breast cancer, are diagnosed and treated, offering faster, less invasive, and more personalised care.
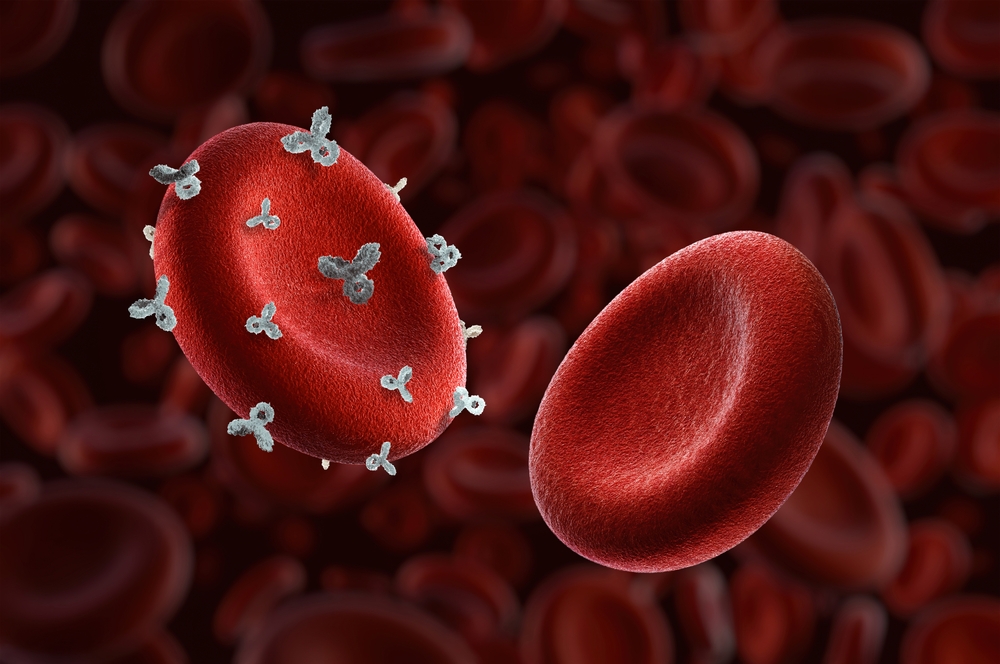
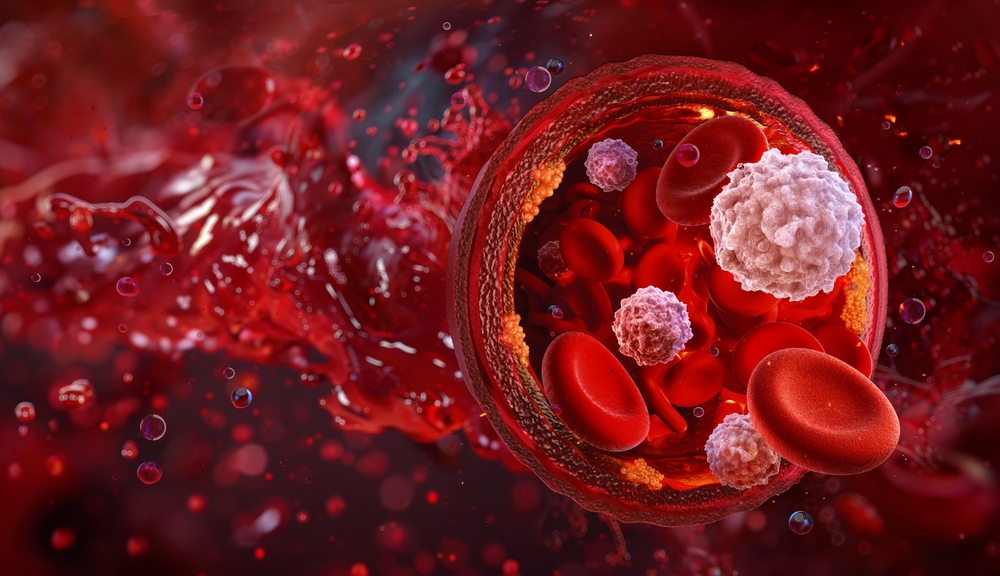
Unlike traditional biopsies that often require surgery or needle-based tissue extraction, liquid biopsies identify fragments of tumour DNA circulating in the bloodstream. This allows clinicians to determine the most effective targeted therapies without putting patients through physically demanding or high-risk procedures. Backed by a successful pilot and poised to benefit up to 20,000 patients annually, this rollout is more than a technological advance. It’s a milestone in how public health systems can deliver precision medicine on a national scale.

A Pioneering Shift in Cancer Diagnosis
The NHS has taken a historic step in cancer care by becoming the first national health system in the world to roll out a “liquid biopsy” blood test on a broad scale. This test represents a fundamental shift in how cancers, particularly lung and breast cancers are diagnosed and managed, offering a less invasive, faster, and more personalized alternative to traditional tissue biopsies.
At the heart of the technology is its ability to detect minuscule fragments of tumor DNA known as circulating tumor DNA (ctDNA) present in the bloodstream. These fragments carry genetic mutations specific to a patient’s cancer, which clinicians can analyze to determine the most effective targeted therapies. This molecular-level insight helps accelerate the path to treatment, sometimes reducing wait times by up to two weeks, particularly for patients with non-small cell lung cancer (NSCLC).
Unlike conventional biopsies, which often require surgical procedures or needle extractions that carry risks and discomfort, liquid biopsies only require a simple blood draw. For many patients, this means avoiding painful procedures, faster diagnosis, and in some cases, being spared from receiving chemotherapy when it’s not needed. As Professor Peter Johnson, NHS National Clinical Director for Cancer, noted, this development signals a “new era of personalised care”, offering not only precision but also compassion in treatment planning.
The test’s initial rollout has already benefited over 2,000 patients since April, with expectations that up to 20,000 people annually including 15,000 lung cancer patients and 5,000 women with advanced breast cancer will be eligible. Beyond its current use, researchers are exploring its potential in other hard-to-detect cancers like pancreatic and gallbladder, positioning the liquid biopsy as a cornerstone of future oncology.

From Pilot to Policy — Building on Real-World Evidence
The NHS’s decision to expand the use of liquid biopsy tests nationally was grounded in a substantial pilot program involving around 10,000 patients with non-small cell lung cancer (NSCLC). This trial provided critical real-world evidence demonstrating the test’s clinical and logistical effectiveness. One of the most significant findings was the test’s ability to reduce the time it takes for patients to begin targeted treatment by up to two weeks. In cancers like NSCLC, where disease progression can be rapid, this time-saving is more than a matter of efficiency; it directly contributes to better prognoses and survival outcomes.
The pilot also highlighted the benefits of moving away from one-size-fits-all treatments toward precision medicine. By detecting genetic mutations in circulating tumor DNA, clinicians were better equipped to prescribe therapies specifically designed for each patient’s cancer profile. This not only improved the chances of treatment success but also spared many patients from unnecessary chemotherapy and invasive biopsies. Avoiding such procedures can significantly enhance quality of life, reducing both physical discomfort and emotional strain. In many cases, the liquid biopsy offered a path to quicker decisions with fewer risks, a shift especially important for patients who may already be frail or managing multiple health conditions.
Importantly, the pilot also revealed potential cost savings for the healthcare system. An independent analysis estimated that adopting liquid biopsies for lung cancer patients alone could save the NHS up to $13.8 million million annually. These savings stem from fewer hospital stays, reduced reliance on high-cost treatments that may be ineffective for certain patients, and better allocation of clinical resources. The success of the pilot didn’t just prove that the test worked; it showed that it worked within the complex ecosystem of NHS care, justifying its broader rollout not only from a medical perspective but also from an economic and operational one.
Putting Patients First — Faster, Kinder, and More Precise Care
For many patients, the journey from suspicion of cancer to treatment can be long, invasive, and emotionally draining. Traditional tissue biopsies, often involving surgery or needle insertion into the lung or other organs, carry risks such as infection, bleeding, and significant discomfort. The new liquid biopsy offers a profoundly different experience requiring only a simple blood draw to provide clinicians with the molecular information they need to plan treatment. This streamlined process reduces not only medical risk but also the psychological burden patients face while awaiting results and decisions.
By identifying genetic mutations directly from a blood sample, clinicians can quickly match patients with targeted therapies designed to interrupt the specific mechanisms driving their cancer. This is especially critical for those with advanced lung or breast cancer, where each day counts and where the wrong treatment can result in avoidable side effects without any real benefit. Avoiding unnecessary chemotherapy, often a blunt, system-wide treatment, means patients experience fewer debilitating side effects like fatigue, nausea, and immune suppression, all of which can dramatically affect quality of life.
The emotional and practical impact of these improvements cannot be overstated. Faster diagnoses and fewer invasive procedures reduce anxiety and allow patients and families to make decisions from a position of clarity and control. As Professor Peter Johnson described, this test represents a “new era of personalised care” where the system adapts to the patient, not the other way around. It empowers individuals to start treatment sooner, suffer less, and maintain more of their daily routines and independence, all of which are essential elements of dignity in care.
A National Milestone with Global Implications
The NHS’s nationwide adoption of liquid biopsy technology represents not only a policy shift but a defining moment in the evolution of cancer care. By becoming the first healthcare system in the world to implement this approach at scale, the NHS is not only delivering tangible improvements for tens of thousands of patients but also setting a precedent for what modern, data-driven medicine can look like in a public health setting. This isn’t an experimental trial or isolated innovation; it’s a system-wide commitment to using genomic data to inform treatment in real time, with infrastructure and protocols that can be replicated across other countries and disease areas.
The move reflects years of investment in genomic capability and a deliberate shift toward precision medicine, where care is informed not just by where a tumor is located, but by its underlying biology. By detecting cancer-related mutations through circulating tumor DNA, clinicians can make decisions that are far more nuanced than traditional pathology allows. The rollout also underscores the NHS’s ability to integrate cutting-edge science into everyday clinical practice bridging the gap between laboratory research and bedside care. This alignment between science, policy, and delivery is rare and critical in advancing equitable access to innovation.
Moreover, the implications go beyond lung and breast cancer. With research already underway to explore the use of liquid biopsies in pancreatic and gallbladder cancers both of which are notoriously difficult to diagnose early. This technology could reshape how a wide range of cancers are detected and managed. In doing so, the NHS is charting a course that others are likely to follow: demonstrating that with the right commitment, personalised medicine can be both scalable and cost-effective within a national health service. The goal isn’t simply to lead but to demonstrate how innovation can serve the principles of public health.
Looking Ahead — Personalised Medicine as a Public Health Imperative
The national rollout of the liquid biopsy test represents not only a clinical advance but also a clear statement of intent about the future of healthcare. At a time when health systems around the world are under pressure to do more with less, the NHS’s adoption of this precision-driven tool shows that innovation and equity are not mutually exclusive. This is healthcare evolving in the direction it must go: faster, more personalised, and less invasive not only to improve outcomes but to respect the lived experience of each patient.
But breakthroughs like this do not sustain themselves without continued investment, public awareness, and a commitment to data-driven care. As more patients gain access to personalised therapies through genomic testing, it becomes even more important to ensure that diagnostic tools are available across all communities, and that clinicians are trained to interpret and act on complex molecular data. Policymakers, health professionals, and patients alike have a role to play in advocating for technologies that make medicine smarter and more humane.
The success of the liquid biopsy rollout is a reminder of what is possible when innovation serves the public good. It challenges us to rethink old models of care and to embrace a future where earlier detection, targeted treatment, and reduced suffering are not the exception but the standard. For someone hearing the word “cancer,” the promise isn’t only quicker answers. It’s compassion, a kind of care that remembers the person within the diagnosis.
Some of the links I post on this site are affiliate links. If you go through them to make a purchase, I will earn a small commission (at no additional cost to you). However, note that I’m recommending these products because of their quality and that I have good experience using them, not because of the commission to be made.




























 JOIN OVER
JOIN OVER
Comments