Highly Contagious Stomach Virus Cases Double in the Midwest Ahead of Holidays
Last updated on
Something uninvited arrived at America’s doorstep weeks ahead of schedule. While families prepare for holiday gatherings and year-end celebrations, a different kind of guest has been making the rounds across the Midwest and Northeast. Wastewater systems tell a story that clinical data alone cannot capture, and what they reveal demands attention. Medical facilities across Indiana, Michigan, and Louisiana report a pattern that infectious disease specialists find concerning. A highly contagious pathogen has begun its seasonal march through communities far earlier than historical trends would suggest. Numbers from wastewater monitoring programs paint a picture of accelerating transmission, with contamination levels climbing to heights unseen in years.GII.17 Variant Fuels Unexpected Surge
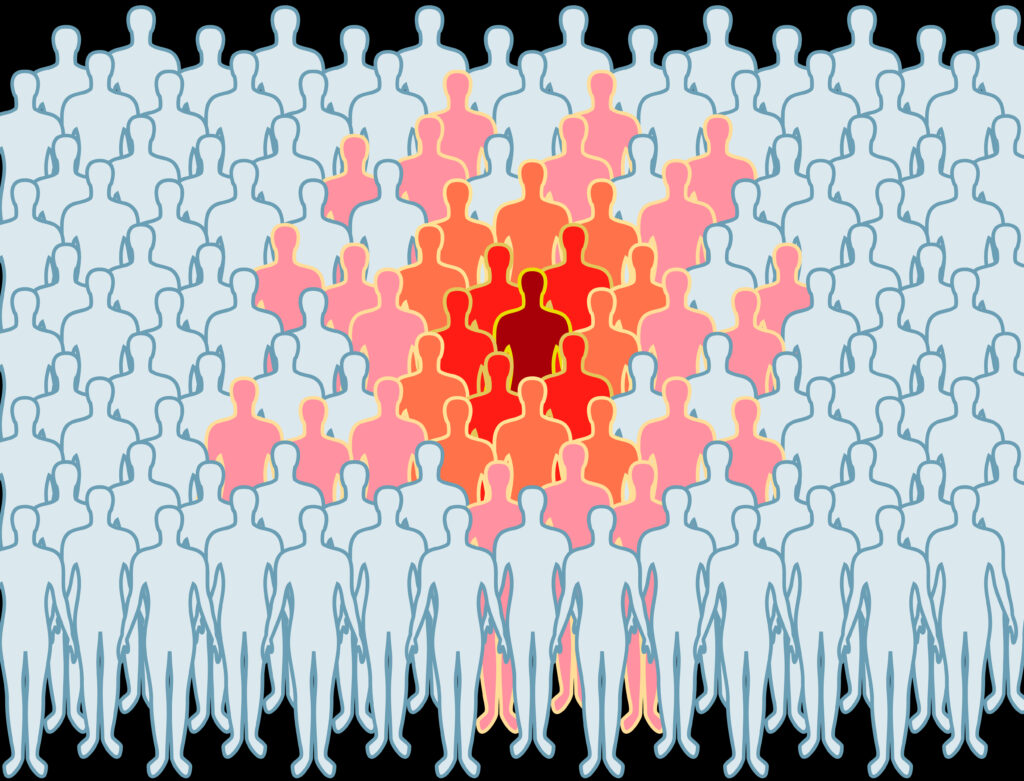
Norovirus, often called winter vomiting disease, has shifted its behavior. A variant designated GII.17 now drives three-quarters of all outbreaks, a dramatic change from 2023 when it accounted for less than 10% of cases. For over three decades, a different strain called GII.4 dominated the norovirus scene. That era appears to be ending. Dr. Robert Atmar, professor in the Department of Medicine at Baylor College of Medicine, explained the shift. “The two possibilities is that something in the virus changed to make it more transmissible, or there were changes in the population that a larger proportion were susceptible,” he noted. “And probably it’s a combination of both.” GII.17 has gained ground across several countries throughout the 2020s. Scientists debate whether the variant carries enhanced transmissibility or simply exploits a population lacking immunity to its specific characteristics. Either way, communities face a pathogen that many immune systems have never encountered before. Mid-October marked the beginning of increased activity, weeks before the typical winter surge. Experts studying viral evolution and population immunity cannot yet predict whether GII.17 will maintain its dominance or whether the older GII.4 strain might reassert itself. What remains clear is that the earlier onset has caught many off guard.Wastewater Data Reveals Regional Hotspots
Cases Double Within Weeks
Test positivity rates tell a compelling story. Around 14% of norovirus tests came back positive during the week of November 15, double the roughly 7% positivity recorded three months earlier. By the first week of December, at least 91 outbreaks were reported, more than double the maximum number documented during the same timeframe in previous years. December 2024 set records, with test positivity hitting almost 25%. After that peak, positivity rates declined gradually through the following months. Now, numbers climb again. Between August 1 and November 13, health departments participating in the CDC’s NoroSTAT program reported 153 outbreaks. Wastewater monitoring reveals cases that never appear in official tallies. Most people who contract norovirus never visit a doctor or receive testing. They suffer at home, recover, and move on. Wastewater surveillance captures their infections anyway, providing early warning signals that clinical data alone cannot offer.Symptoms Hit Fast and Fierce

20 Million Annual Infections Make Norovirus America’s Top Foodborne Illness
Each year, norovirus causes approximately 19 to 21 million illnesses across the United States. It stands as the leading cause of gastroenteritis, an inflammation of the gastrointestinal tract. More than half of all foodborne illnesses in America trace back to this single pathogen. Hospitals admit about 109,000 people annually due to norovirus complications. Roughly 900 deaths occur each year. While most healthy adults recover fully, the very young and very old face considerably higher risks. Children under five and adults over 85 require careful monitoring. Norovirus is a human-only disease. It does not infect animals or spread through animal contact. Person-to-person transmission drives nearly all outbreaks. Once it enters a community, it moves quickly through households, schools, nursing homes, and other congregate settings.Perfect Pathogen Survives Extreme Conditions
Multiple Transmission Routes Speed Spread
Norovirus spreads through numerous pathways. Direct contact with infected individuals represents the most common route. Touching contaminated surfaces and then touching the mouth transmits the virus efficiently. Food and water contaminated during preparation or processing cause frequent outbreaks. Aerosolized particles from vomit create another transmission vector. When someone vomits, tiny droplets become airborne. People nearby can inhale these particles, or they can settle on surfaces. Cleaning up after an infected person requires specific protocols to prevent further spread. Shellfish, particularly oysters and clams, concentrate norovirus from their environment. As filter feeders, they accumulate viral particles from untreated sewage that flows into their habitats. Raw or undercooked shellfish consumption carries substantial risk during outbreak periods.Hand Sanitizer Fails Against Norovirus

No Treatment Exists Beyond Symptom Management
Stay Home 48 Hours After Symptoms End
Isolation remains one of the most effective control measures. People who contract norovirus should stay home for at least 48 hours after their symptoms resolve. During recovery and the extended contagious period afterward, infected individuals should avoid preparing food for others. Proper food handling reduces risk. Shellfish must be cooked to the appropriate temperatures. Fruits and vegetables require thorough washing. Anyone who feels even slightly unwell should not work in food service or prepare meals for groups. As wastewater contamination levels continue rising and holiday celebrations bring people together, awareness becomes essential. Norovirus may lack the dramatic profile of pandemic threats, but its annual toll remains substantial. Communities across the Midwest and Northeast face a season that started early and shows no signs of slowing down. Featured Image Source: Wikimedia CommonsView this post on Instagram
Some of the links I post on this site are affiliate links. If you go through them to make a purchase, I will earn a small commission (at no additional cost to you). However, note that I’m recommending these products because of their quality and that I have good experience using them, not because of the commission to be made.

































 JOIN OVER
JOIN OVER
Comments