A Bacterial Cause of Endometriosis Emerges Alongside a Potential Therapy
Last updated on
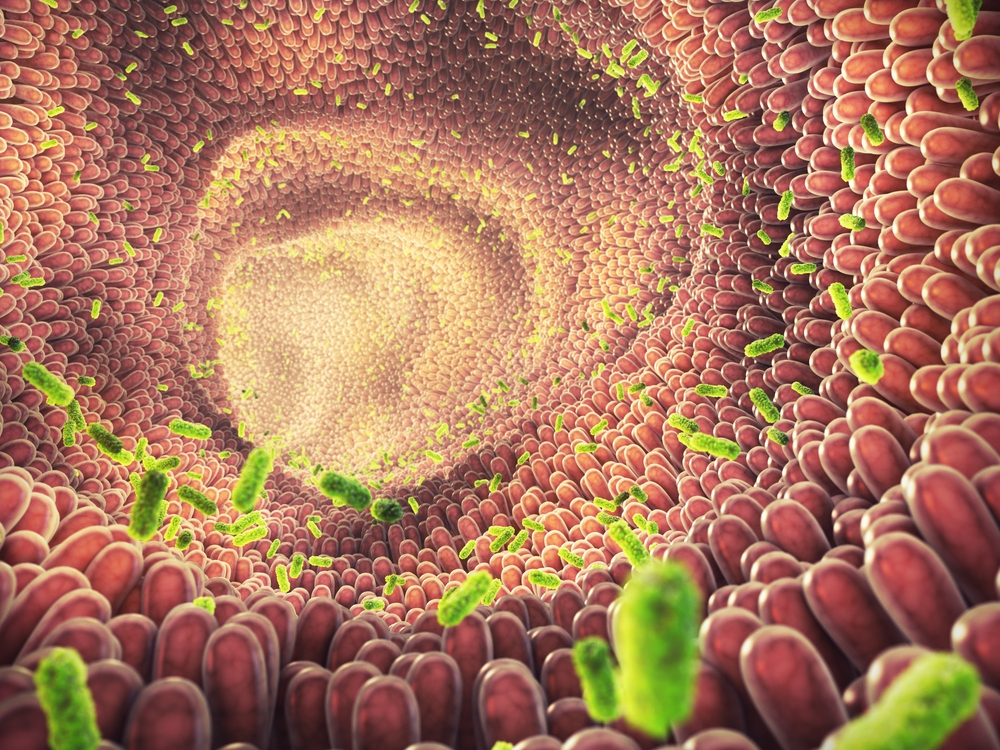
Endometriosis has long been a medical mystery, leaving millions of women to navigate a maze of chronic pain with treatments that often force a difficult choice between relief and fertility. This status quo of hormonal suppression and invasive surgeries may finally be crumbling. New research challenges the traditional understanding of the disease, pointing to a surprisingly common bacterial culprit and raising the possibility of a cure that treats the cause rather than just the symptoms.The Link Between Bacteria and Endometriosis
Endometriosis affects roughly one in 10 women of reproductive age, often causing debilitating pelvic pain and infertility. Despite its prevalence, patients frequently face an agonizing eight-year delay in diagnosis. For decades, the leading theory for the cause has been “retrograde menstruation,” where menstrual blood flows backward into the pelvic cavity. However, this theory has a significant flaw: while many women experience retrograde menstruation, only a fraction develop endometriosis. This discrepancy has puzzled the medical community, suggesting a missing piece in the puzzle. A breakthrough study from Nagoya University in Japan provides a compelling answer. Led by Professor Yutaka Kondo and Assistant Professor Ayako Muraoka, the research team identified a specific bacterial infection, Fusobacterium, as a likely culprit. In their analysis of tissue samples from 155 women, they found that 64% of patients with endometriosis carried this bacterium in their uterine lining. In sharp contrast, fewer than 10% of the healthy control group tested positive. This finding suggests that bacterial infection may be the key event that triggers the disease in susceptible individuals. Professor Kondo highlighted the significance of this shift, stating, “Our data provide a strong and novel rationale for targeting Fusobacterium as a non-hormonal antibiotic-based treatment for endometriosis.” This discovery fundamentally changes the conversation, moving the focus from purely hormonal management to potentially treating the root cause with antibiotics.How Bacteria Drives the Disease

A Potential Cure: Antibiotics Over Hormones

The Path Forward: Validating the Findings

A New Paradigm for Women’s Health

- Muraoka, A., Suzuki, M., Hamaguchi, T., Watanabe, S., Iijima, K., Murofushi, Y., Shinjo, K., Osuka, S., Hariyama, Y., Ito, M., Ohno, K., Kiyono, T., Kyo, S., Iwase, A., Kikkawa, F., Kajiyama, H., & Kondo, Y. (2023b). Fusobacterium infection facilitates the development of endometriosis through the phenotypic transition of endometrial fibroblasts. Science Translational Medicine, 15(700), eadd1531. https://doi.org/10.1126/scitranslmed.add1531
- Muraoka, A., Suzuki, M., Hamaguchi, T., Watanabe, S., Iijima, K., Murofushi, Y., Shinjo, K., Osuka, S., Hariyama, Y., Ito, M., Ohno, K., Kiyono, T., Kyo, S., Iwase, A., Kikkawa, F., Kajiyama, H., & Kondo, Y. (2023b). Fusobacterium infection facilitates the development of endometriosis through the phenotypic transition of endometrial fibroblasts. Science Translational Medicine, 15(700), eadd1531. https://doi.org/10.1126/scitranslmed.add1531
Some of the links I post on this site are affiliate links. If you go through them to make a purchase, I will earn a small commission (at no additional cost to you). However, note that I’m recommending these products because of their quality and that I have good experience using them, not because of the commission to be made.

































 JOIN OVER
JOIN OVER
Comments