Woman, 30, Diagnosed With Brain Tumor After Telling Her Doctor About Common Symptom
Last updated on
What if the sound that’s been quietly following you for years a faint whoosh in your ear, a hum you barely notice anymore turned out to be the reason you’re still alive? Most of us shrug off small bodily quirks: a twitch in the eyelid, a twinge in the knee, a dull headache that comes and goes. They’re part of being human, easily blamed on stress, long workdays, or poor sleep. But sometimes, a symptom that feels forgettable can be the breadcrumb leading to something far bigger.
Brain tumors are rare affecting only about 5 in every 100,000 people each year yet they can grow in silence, pressing against delicate neural pathways long before showing their hand. For Paige Footner, a 30-year-old paramedic and circus performer from Australia, it wasn’t blinding headaches or sudden weakness that sent her to the doctor. It was a persistent sound in one ear she’d lived with for four years.
She didn’t know it yet, but that small act of speaking up would change everything.
Understanding Brain Tumors
The word tumor often sparks immediate fear, while the word benign can bring a sigh of relief. In the context of brain health, though, the reality is more complicated. Even when a tumor is non-cancerous, its presence inside the confined space of the skull can still threaten a person’s wellbeing.
A brain tumor is an abnormal growth of cells within the brain or in the tissues surrounding it, such as the meninges the protective layers covering the brain and spinal cord. Tumors can be primary, meaning they originate in the brain, or secondary (metastatic), meaning cancer from another part of the body has spread to the brain. There are more than 150 known types of brain tumors, each with unique behaviors, growth rates, and treatment challenges.
In Paige’s case, doctors suspected a meningioma, a primary tumor that typically grows slowly and is most often benign. Meningiomas account for roughly one-third of all primary brain tumors. They are more common in women, especially over the age of 60, but can appear at any stage of adulthood. While many grow quietly for years without causing symptoms, their impact is determined by where they develop.
That’s because the brain is enclosed in a rigid, bony structure with no extra space. Even a small, slow-growing mass can press on areas that control vision, balance, speech, memory, or personality. This pressure can lead to problems such as:
- Persistent headaches, especially in the morning
- Seizures
- Weakness or numbness on one side of the body
- Vision disturbances
- Cognitive or mood changes
These symptoms don’t distinguish between benign and malignant tumors they arise from the tumor’s location and the pressure it creates. A benign meningioma sitting near the motor cortex could impair movement just as much as a malignant tumor in the same spot.
According to the American Cancer Society, the lifetime risk of developing any brain or spinal cord tumor malignant or benign is less than 1%. But when they do occur, early detection can make the difference between straightforward treatment and life-altering complications. The challenge? Many tumors remain silent until they’re large enough to cause noticeable changes.
The Role of Imaging and Medical Persistence in Saving Lives

When Paige Footner agreed to an MRI scan, it wasn’t because she suspected a tumor. Her doctors didn’t either. The test was ordered as a precaution to rule out structural causes for her tinnitus before she left for an international performance tour. In the end, it was that willingness to follow through that made the invisible visible.
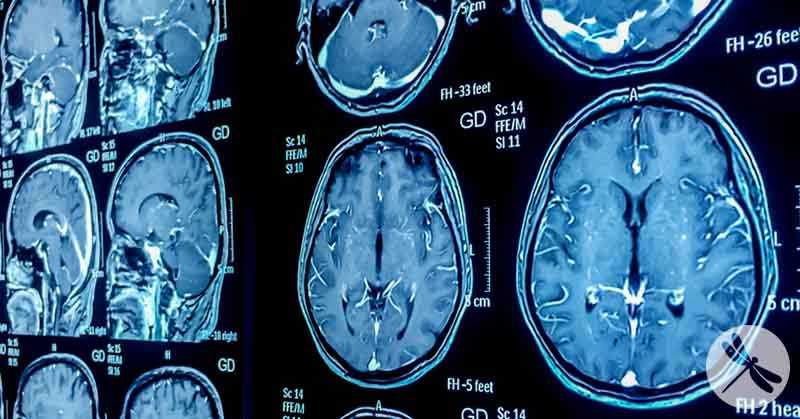
Magnetic Resonance Imaging (MRI) is one of the most powerful tools for examining the brain. Unlike X-rays or CT scans, which use radiation, MRI relies on magnetic fields and radio waves to create detailed images of soft tissue. This clarity makes it ideal for detecting subtle abnormalities, such as small lesions, changes in tissue density, or growths hidden deep within the brain’s folds.
The tumor in Paige’s posterior right frontal lobe might never have been found without that scan. It was an incidental finding a medical discovery unrelated to the patient’s original concern. Such findings are not uncommon in neurology. MRIs ordered for chronic headaches, dizziness, or even after minor head injuries sometimes uncover aneurysms, vascular malformations, or tumors that were producing no symptoms at all.
In the case of brain tumors, this kind of early detection can drastically change the outcome. Tumors found before they cause neurological deficits are often smaller, more accessible for surgical removal, and less likely to have caused permanent damage. Once symptoms like seizures, vision loss, or personality changes appear, the tumor has often grown large enough to affect surrounding tissue, making surgery more complex and recovery more uncertain.
That doesn’t mean every persistent symptom calls for an MRI. Most cases of tinnitus, for example, are caused by non-threatening issues such as noise exposure or age-related hearing changes. But medical experts emphasize the importance of patterns: symptoms that are one-sided, worsening, or unexplained over time should prompt a closer look.
Paige’s case demonstrates why persistence matters. She didn’t request advanced testing out of fear she did it to be thorough. And that diligence caught a tumor before it could announce itself in far more dangerous ways. As her neurosurgeons told her, she was “so lucky” to have found it when she did.
The Human Cost of a Diagnosis

The MRI results came just weeks before Paige Footner was meant to board a flight to Scotland a trip she had meticulously planned and financed to showcase her talents at the Edinburgh Fringe Festival. She had trained relentlessly, balancing circus rehearsals with demanding shifts as a paramedic. Flights and accommodation were booked, performance slots secured, and $13,000 already charged to her credit card. She hadn’t yet purchased travel insurance.
In a single phone call, that world collapsed. The trip was cancelled. Instead of performing on a world stage, she was scheduling surgery consults and undergoing PET scans to assess whether the tumor had spread. While doctors suspected a slow-growing meningioma, certain irregular features raised the possibility of something more aggressive. Surgery was not optional.
The practical fallout was immediate and heavy. Post-operative driving restrictions meant Paige could not work as a paramedic for at least six months a significant loss of income. Performing in the circus, a physically demanding art form requiring balance, strength, and coordination, was also out of the question during recovery. The debt from her cancelled trip remained, now joined by medical bills.
But beyond finances, the emotional toll was profound. Known in circus circles for her fearlessness and precision, Paige suddenly felt vulnerable in a way no high-stakes performance had ever made her feel. “I felt vulnerable and scared and weak,” she admitted emotions at odds with the grit and control she had built her career on.
Some fears cut deeper than the diagnosis itself. “My first thought when they told me was, ‘I’m going to die, and I’ve never been in love.’” It was an intimate, human reckoning the realization that some of life’s most personal milestones might never be reached.
Initially, Paige kept the news private, telling only her boss. But he encouraged her to share her story, believing that the support of her community could help her through the months ahead. He was right. Messages poured in from friends, colleagues, and strangers, many sharing how she had touched their lives. That response reframed her perspective.
“I didn’t know how much of a difference I’d made in people’s lives until now,” she said. “I guess I’ve achieved my purpose in life.” In the space between loss and uncertainty, Paige found an unexpected anchor: the knowledge that her work and presence had mattered more than she realized.
Listening to Your Body

Paige’s story isn’t about panic it’s about paying attention. The whooshing in her ear wasn’t painful, disabling, or urgent. But it was different, persistent, and one-sided three characteristics doctors often cite as worth investigating. Her decision to bring it up during a routine appointment, and to follow through with specialist referrals, may have saved her life.
For most of us, the challenge isn’t recognizing symptoms; it’s deciding when they matter enough to act on. Many common issues headaches, dizziness, fatigue, tinnitus are usually harmless. But when they change, linger, or feel unusual, they deserve a closer look. Here’s how to tune in without spiraling into alarm:
1. Don’t Dismiss Persistent Symptoms If something is one-sided (like unilateral tinnitus), ongoing for more than a few weeks, or gradually getting worse, talk to your doctor. Be specific about when it started, how often it happens, and what makes it better or worse.
2. Keep a Simple Symptom Log A few notes in your phone can make a big difference. Dates, times, triggers, and severity help your doctor spot patterns you might miss.
3. Follow Through on Referrals and Tests Life gets busy, and it’s easy to postpone non-urgent appointments. But delayed imaging or specialist visits can close the window for early detection.

4. Ask Questions And Get a Second Opinion if Needed You’re not being difficult by asking why a test is ordered, what the next steps will be, or whether there are other possibilities to consider. Another medical opinion can provide reassurance or reveal new insights.
5. Be Honest About Your Lifestyle and Risks Your daily activities, injuries, and stress levels help guide medical decisions. In Paige’s case, her career in circus performance initially seemed a likely cause of her ear symptoms but full context led to further investigation.
6. Trust the Signal, Not Just the Symptom Symptoms are the body’s language. Even if a particular sign turns out to be harmless, it can still point doctors toward something important. Paige’s tinnitus had nothing to do with her tumor but it was the reason she got an MRI in the first place.
Listening to your body isn’t about living in fear. It’s about knowing when curiosity, persistence, and a bit of self-advocacy can tip the balance between a silent threat and a survivable outcome.
Trust the Signal, Not Just the Symptom
Paige Footner’s diagnosis didn’t come from a flashing warning sign it came from a quiet, persistent symptom that had become part of her everyday life. She didn’t demand answers in panic, nor did she ignore it out of convenience. Instead, she followed a simple but powerful instinct: to mention it, to follow through, and to stay curious enough to seek clarity.
Her story is a reminder that health isn’t just about reacting to crises it’s about respecting the subtle messages your body sends you. Most of those messages will lead nowhere serious, but sometimes, as in Paige’s case, they open a door to life-saving intervention.
You don’t need to be a medical professional or an elite performer to take your health seriously. You just need the willingness to pause, listen, and ask, “Could this be something?” Early action doesn’t always guarantee a better outcome but it often creates the chance for one.
In the end, Paige’s path to treatment began not with a grand medical discovery, but with a conversation. And sometimes, that’s all it takes to change the story.
Some of the links I post on this site are affiliate links. If you go through them to make a purchase, I will earn a small commission (at no additional cost to you). However, note that I’m recommending these products because of their quality and that I have good experience using them, not because of the commission to be made.




























 JOIN OVER
JOIN OVER
Comments