Man Took 40,000 Ecstasy Pills in His Twenties and Now Lives With Severe Physical and Mental Damage
Last updated on
If you swallowed one pill of ecstasy every single day, it would take you over a century, 109 years to be exact, to reach a total of 40,000. One man did it in less than a decade.
Known only as “Mr. A,” this British man’s drug use began in the familiar glow of weekend parties and warehouse raves, but quickly spiraled into something far more harrowing. By the end of his twenties, he was consuming 25 ecstasy tablets a day, an amount so staggering that doctors called his case the most extreme ever recorded.
What followed was not just a hangover, but a near-complete collapse of mental clarity and physical stability. Memory loss, hallucinations, paranoia, and neurological dysfunction became his new normal, long after the drugs had left his system.
From Weekend Highs to Daily Despair

Mr. A’s descent into extreme drug use didn’t begin with reckless abandon. It began, like many others’, in the glow of a youth culture that normalized weekend experimentation. At 21, he started taking ecstasy (MDMA) casually, averaging five tablets per weekend as part of the UK’s vibrant club scene. But over the next nine years, what began as a recreational habit turned into a daily ritual of self-destruction.
By 23, Mr. A’s usage had already shifted from weekends to weekdays, with his intake jumping to an average of 3.5 pills a day. By his late twenties, he was ingesting a staggering 25 pills daily. Over the course of nearly a decade, this amounted to a total of approximately 40,000 ecstasy tablets, a quantity so excessive that it dwarfs the previously documented highest known intake of 2,000 pills.
Dr. Christos Kouimtsidis, a consultant psychiatrist who treated Mr. A at St George’s Medical School in London, emphasized just how unusual his case was: “Typical use is not every day and not the amount of tablets he was taking. It was extreme.” In fact, the levels of MDMA in Mr. A’s system were so high that he remained in an altered state for months after quitting, reporting persistent drug-like sensations and visual distortions despite abstinence.
While most users might take ecstasy occasionally for social or euphoric effects, Mr. A’s pattern reflects a transition from use to dependence and ultimately, to a form of chemical self-sabotage. By the time he experienced three separate collapses at parties and decided to stop using, the damage was already deeply entrenched.
Permanent Damage: The Cognitive Collapse of a Heavy User
By the time Mr. A stopped taking ecstasy at age 30, the damage was already in full effect and it didn’t go away when the pills did. In the months following his withdrawal, he reported feeling as if he were still under the influence of the drug, experiencing surreal episodes of tunnel vision and a lingering sense of detachment from reality. These symptoms weren’t common in known cases of MDMA withdrawal, but then again, no one had ever consumed 40,000 pills before.
What unfolded next was a cascade of debilitating mental and physical effects. Mr. A developed severe panic attacks, recurrent anxiety, depression, and paranoid ideation. He experienced functional hallucinations not fleeting visuals, but vivid misperceptions that interfered with his daily functioning. A recurring symptom was muscle rigidity, especially in the neck and jaw, a known side effect of ecstasy due to its impact on dopamine and serotonin regulation in the brain.
The damage to his cognitive function was among the most alarming. Psychological assessments revealed that while Mr. A could understand instructions, his short-term memory and concentration were so impaired that he was unable to complete even basic sequences of tasks. He also suffered from disorientation to time, forgetting the day, the hour, or what he had just done. According to his doctors, the severity of his short-term memory issues resembled that of a lifetime alcoholic, despite no history of alcohol dependency.
Perhaps even more concerning was Mr. A’s lack of insight into his condition. Dr. Kouimtsidis noted that he “did not seem aware himself that he had these memory problems,” a phenomenon known as anosognosia, often seen in patients with brain injury or severe cognitive decline.
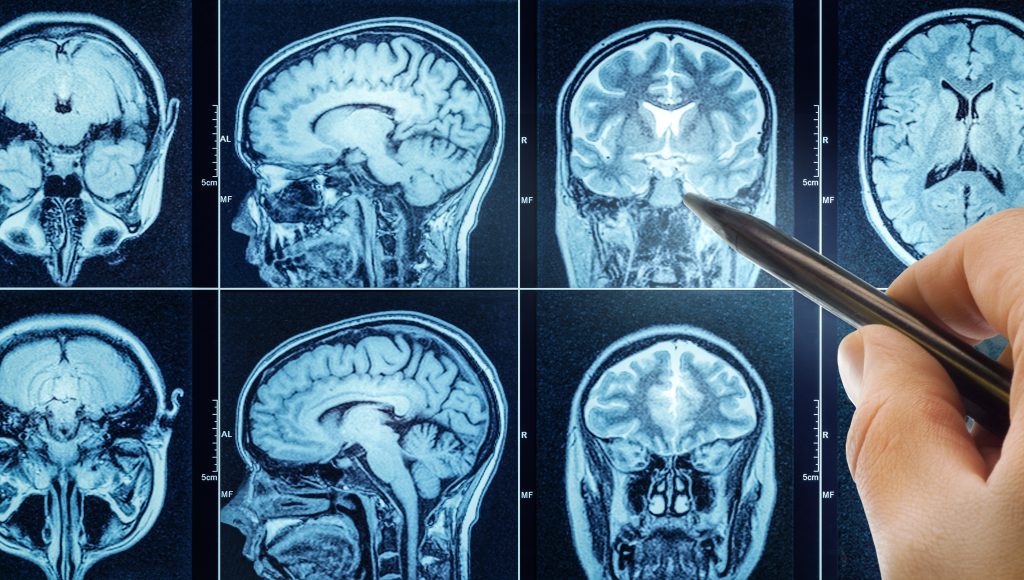
Brain imaging, however, failed to reveal clear structural damage. An MRI scan showed no obvious atrophy or lesions, a reminder of how difficult it can be to correlate visible brain changes with functional impairments, especially when current technology lacks the sensitivity to detect all forms of neurotoxicity. Some improvement was observed when Mr. A was admitted to a brain injury unit and placed on antipsychotic medication, but he ultimately discharged himself before completing treatment.
Complicating the picture was Mr. A’s heavy cannabis use, which appeared to intensify symptoms like paranoia and hallucinations. When he reduced his cannabis intake, those particular issues improved. However, his memory deficits and concentration problems persisted, suggesting that these impairments were likely tied to the long-term, high-dose MDMA exposure rather than any secondary drug use.
Risks, Limits, and Unknowns

MDMA, also known as ecstasy or “Molly,” is one of the most studied recreational drugs globally. Despite its widespread use and growing popularity as a potential therapeutic tool, the scientific consensus on its long-term effects remains unclear, particularly regarding high-dose or chronic use. Mr. A’s case, though extreme, serves as a stark reminder of how much we still don’t know about the drug’s impact on the brain and body, and why it’s so crucial to approach its use with caution.
At the chemical level, MDMA primarily affects three neurotransmitters: serotonin, dopamine, and norepinephrine. The surge in serotonin is what creates MDMA’s signature effects like euphoria, emotional warmth, and a distorted sense of time. Serotonin plays a significant role in mood regulation, memory, and sleep, so its depletion through repeated or excessive use can lead to a range of negative outcomes. This depletion has been linked to depression, anxiety, and memory problems, which can worsen over time with continued use.

The NHS highlights that regular MDMA use can disrupt the balance of serotonin in the body, leading to psychological issues such as low mood, sleep disturbances, and long-term emotional instability. These effects are often most intense during the withdrawal phase, and for heavy users, they can evolve into clinical depression or panic disorders. The long-term psychological toll can be severe, particularly for those who engage in frequent or high-dose use, like Mr. A.
In more extreme cases, such as Mr. A’s, scientists suspect that excessive MDMA use may cause neurotoxicity, a toxic effect on nerve cells, especially in the serotonin system. However, proving this damage is challenging. For example, a structural MRI of Mr. A’s brain showed no clear abnormalities, leading experts to point out the limitations of current brain imaging technology. As Dr. Kouimtsidis explained, these scans are “not sensitive enough” to detect subtle damage to neurotransmitter systems or neural pathways. This uncertainty is one of the key challenges in MDMA research, leaving scientists divided on the long-term effects of the drug.
Can a Dangerous Party Drug Also Heal Trauma?

MDMA has recently gained attention for its potential in enhancing psychotherapy, particularly for PTSD. In controlled, therapeutic settings, the drug appears to help patients access and process traumatic memories without the overwhelming fear or emotional shutdown that often hinders traditional therapy. By boosting serotonin and reducing activity in the amygdala, the brain’s fear center, MDMA fosters emotional openness, self-reflection, and deeper connection.
One of the most promising studies was a Phase 3 clinical trial led by researchers from the University of California, San Francisco, and New York University. In this randomized, placebo-controlled trial, 88% of participants with severe PTSD saw significant symptom relief following MDMA-assisted therapy. The rigor of this study, including double-blind procedures and careful oversight, marks a breakthrough in psychedelic research and could reshape how MDMA is viewed and regulated in the future.
However, clinical trials are worlds apart from recreational use. In therapeutic settings, participants undergo careful screening, doses are precisely measured, and experienced therapists provide guidance throughout the experience. MDMA is administered a few times under strict supervision, ensuring a controlled and safe environment, unlike the unchecked use seen in recreational settings.
Mr. A’s story highlights the stark contrast between therapeutic and recreational use. His prolonged, unregulated use of MDMA caused memory loss, emotional instability, and hallucinations, turning what could have been a tool for healing into a source of new trauma. As public interest in MDMA therapy grows, his case serves as a reminder that powerful substances can both heal and harm, underscoring the importance of moderation, oversight, and ethical responsibility in its use.
The Irreversible Cost of Drug Abuse

Mr. A’s story is more than just a statistic. It’s a powerful reminder of what can happen when we push our boundaries and misunderstand the risks of certain substances. His experience may seem extreme, but it’s an important lesson for anyone who’s trying to navigate the blurred lines between recreation, self-medication, and even therapy. His story shows how quickly drug use, which might start as something casual or fun, can spiral into something much darker. The shift from “weekend fun” to daily dependency didn’t happen overnight, but instead crept in slowly, fueled by a culture that often dismisses “party drugs” as harmless.
This is why harm reduction is so important. Instead of just stigmatizing or sensationalizing drug use, we need to focus on honest education. Understanding how substances affect our bodies and brains, being aware of personal risk factors, and learning to spot the early signs that things might be escalating. Not every person who uses drugs becomes addicted, but the further someone pushes their limits, the higher the risk. It’s about striking that balance: knowing when something is just a bit of fun and when it’s crossing into dangerous territory.
Mr. A’s case also shows just how crucial context is. MDMA can be helpful in controlled, clinical settings, where it’s used carefully to help people work through trauma. But when it’s taken in a different context without supervision or medical guidance the same drug can have devastating effects. It’s not about the substance itself, but about how it’s used. The difference lies in the dosage, the supervision, and the intent behind taking it. That’s why it’s so important to be informed and approach these substances with caution, especially if you’re considering them for therapeutic purposes. Knowing the difference between what’s used in a clinical trial and what’s sold on the street could make all the difference in staying safe.
Some of the links I post on this site are affiliate links. If you go through them to make a purchase, I will earn a small commission (at no additional cost to you). However, note that I’m recommending these products because of their quality and that I have good experience using them, not because of the commission to be made.




























 JOIN OVER
JOIN OVER
Comments